Our research focuses on improving the treatment of patients with facial and cranial anomalies. We aim to develop optimal treatment strategies by working synergistically between clinical activities and technological development, as well as biological research as part of the Department of Clinical Research and the Department of Biomedical Engineering at the University of Basel, and through multi-disciplinary local and international collaborations.
Clinical Research
Clinical studies are integral part of our translational research in bridging between recognition of patients needs, emerging technologies from basic research and back to evaluation of its applicability at bedside.
Examples of our studies are:
- Evaluation of treatment strategies conducted in maxillofacial surgery
- Post-operative studies on the effect of cleft lip and palate surgeries
- Psychosocial functioning of patients with facial and cranial anomalies
Technological Advancement
We explore and engage innovative techniques to meet challenges we encounter in our clinical tasks. Areas we have been and are involved include:
- 3D visualization of malformation anomalies
- Use of morphable models to plan facial prosthetics
- Innovative 3D imaging devices for soft tissue surfaces
- 3D printing
- Use of dental magnets for osteogenesis
- Intraoperative integration of robotics and digitalization
Biology
We are involved in research projects aimed to advance our understanding of biological systems and to further explore their application in clinical practices. Examples of current and past projects are:
- Development of stem-cell based products and biomaterials for tissue engineering
- Vascular anatomy upon cleft lip and palate surgery
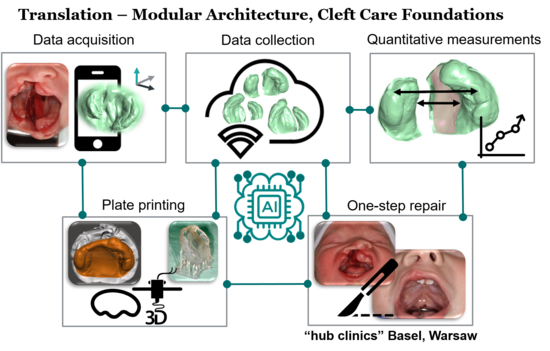
Every 700th birth worldwide is affected by any type of uncompleted development of the upper lip and palatal prominences leading to orofacial cleft (cleft lip and palate). In absence of early surgical correction, main concerns are social discrimination by the disfiguration, nasal leakage of food leading to failure to thrive adequately, and impossibility of speech development. No effective preventive measures exist. Currently, two principles are used and commonly applied complementary as treatment strategies: (1) a palatal plate therapy after birth to keep the tongue out of the cleft space and to narrow the palatal cleft and (2) a multi-step surgical repair. However, this strategy necessitates a palatal impression that endangers the child’s airway and a high surgical burden. The project therefore develops a non-invasive strategy for the palatal plate therapy followed by a one-step surgical repair of the entire cleft lip and palate malformation.
With the use of machine learning algorithms, smartphone-based images of the palate malformation, and 3D printing of tailor-made palatal orthopaedic plates, this project will potentially revolutionise the standard course of treatment of cleft lip and palate. We aim to reduce burden on the patient receiving the cleft lip and palate surgical treatment and to improve the overall long-term outcome. We will exploit our surgical expertise and 3D morphometric knowledges, combined with artificial intelligence to simplify the treatment procedure by developing a ground-breaking new cleft treatment regime:
- Image-based, non-invasive palatal shape reconstruction with the aid of smartphones and a software program based on artificial intelligence
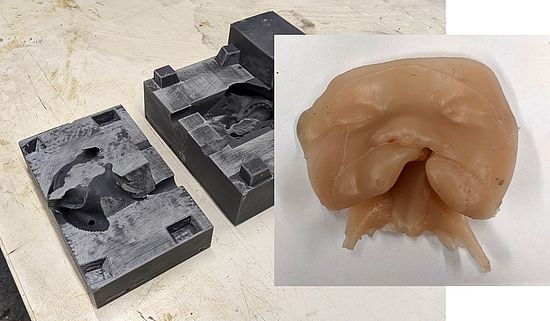
- Use of 3D printing (Zarean et al. 2022) following the automated palatal plate design (Schnabel et al. 2023) to simplify the production process
- Replace multiple surgical steps with one single surgical intervention through use of the palatal plate (passive plate therapy)
Achieving these goals would provide us with a passive, pre-surgical treatment that is physically, technologically and economically realizable worldwide including in low- and middle-income countries, therefore ultimately enable promotion of single-step surgical treatment to replace the widely performed multi-step surgical treatment which impose large burden on the children and their families.
Funding: Burden Reduced Cleft Care and Healing, The Basel Research Centre for Child Health, Multi-Investigator Project 2020-2025
Schnabel TN, Gözcü B, Gotardo P, Lingens L, Dorda D, Vetterli F, Emhemmed A, Nalabothu P, Lill Y, Benitez BK,Mueller AA, Gross M, Solenthaler B. Automated and data-driven plate computation for presurgical cleft lip and palate treatment. Int J Comput Assist Radiol Surg. 2023 Apr 2. doi: 10.1007/s11548-023-02858-6
Zarean P, Zarean P, Thieringer FM, Mueller AA, Kressmann S, Erismann M, Sharma N, Benitez BK. A Point-of-Care Digital Workflow for 3D Printed Passive Presurgical Orthopedic Plates in Cleft Care. Children. 2022; 9(8):1261. https://doi.org/10.3390/children9081261
Collaborators:
Prof. Dr.-Ing. Markus Gross, Computer Graphics Laboratory ETH Zurich & Disney Research Laboratory Zurich
Prof. Dr. sc. Barbara Solenthaler, Simulation and Animation at Computer Graphics Laboratory, ETH Zurich
Prof. Dr. Srinivas Gosla Reddy, G.S.R. Institute of Craniofacial and Facial Plastic Surgery, Hyderabad, India
Assistent Professor Andrzej Brudnicki, Institute of Mother and Child, Department of Surgery of Children and Adolescents, Warsaw, Poland
The aim of cleft lip and palate repair is to normalize the disturbed anatomy and function, concerned mainly with the design of the skin incisions, how the muscle portions are reconstructed and how the nasal and palatal frameworks are repositioned. However, the vascular anatomy has not received much attention in current surgical techniques, despite its crucial role for development and growth.
We are interested in understanding the blood circulation in cleft lip and palate upon surgery in order to improve the recovery and long-term outcome of the surgical treatment.

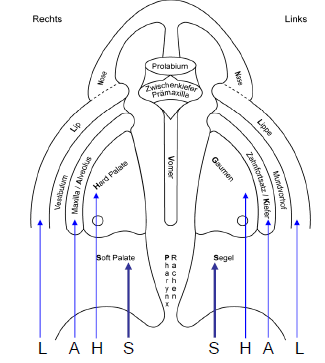
Sites where the blood circulation was measured. At the points marked by open circles, the microcirculatory flow, oxygen saturation, and hemoglobin levels were measured. At the points marked by filled rectangles, the flow velocity in the underlying artery was measured. Corresponding sites were measured before and after surgery in unilateral and bilateral cleft lips and in healthy controls.
Our study on the blood circulation upon lip surgery has shown that there is no intrinsic circulatory deficit in unilateral and bilateral cleft lip-cleft palate patients compared to healthy controls.
Mueller AA, Schumann D, Reddy RR, Schwenzer-Zimmerer K, Mueller-Gerbl M, Zeilhofer HF, Sailer HF, Reddy SG. Intraoperative vascular anatomy, arterial blood flow velocity, and microcirculation in unilateral and bilateral cleft lip repair. Plast Reconstr Surg. 2012;130(5):1120-1130. doi:10.1097/PRS.0b013e318267d4fb
Currently we are conducting a clinical trial to investigate the influence of cleft surgery on the tissue microcirculation of the palate with a non-invasive measurement. We aim to quantify the impact of our surgical technique with minimized incision ouline which allow preservation of major blood vessels and anastomoses to the lip and nose, on the palatal tissue microcirculation. (https://www.clinicaltrials.gov/ct2/show/NCT03877666)

In patients with complete unilateral cleft lip and palate deformities, the bony maxilla (alveolar process) which holds the teeth, is split. Alveolar bone grafting has to be performed to close possible oronasal fistulae and re-establish the continuity of the maxillary alveolar process in order to give a solid bone support and to enable the eruption of permanent teeth in the former cleft area. Sufficient bone stock for the former cleft area is a prerequisite for subsequent orthodontic treatment to align the teeth. Additionally, sufficient bone stock allows harmonious lip and nose soft tissue support for an aesthetic improvement. There are timing issue for alveolar bone grafting. Primary alveolar bone grafting is performed simultaneously with cleft lip or cleft palate repair between birth and the age of 2 years. On the other hand, secondary alveolar bone grafting takes place later. Common sources of autogenous bone grafts are the iliac crest and the mandibular symphysis. Due to the same ectomesenchymal origin as the maxilla, mandibular grafts show excellent bone incorporation. Furthermore, there is no visible scar at the donor site and the operation time can be reduced due to working in the same operating area. The disadvantage using a bone graft from the mandibular symphysis is the limitation of the volume. The availability of large amounts of cancellous and cortical bone as well as easy access are advantages of bone harvest from the iliac crest. The disadvantage of using autogenous bone from the iliac crest alone is the inevitable bone resorption and donor site morbidity. To compensate the graft volume, slowly degradable bone substitute material like micro-structured ß-Tricalcium Phosphate can be used.
In order to accurately evaluate the success of alveolar bone grafting, we explore methodologies and develop a protocol to measure the bone volume, the stability and the resorption rate of the augmented bone. We find that three-dimensional evaluation based on computer tomography or cone beam computer tomography data sets to be suitable choices.
Cleft Lip and Palate Surgery Simulator (CLAPS) - Open Source Simulation Model
The project aims to develop an innovative open source simulator for cleft lip and palate surgery. We have launched a collaborative effort in the framework of a bilateral transboundary research cooperation with a Surgical Oncology and Maxillofacial Surgery Department of Medicine School at Pontifical Catholic University in Chile to ensure direct knowledge transfer.
Supported by Universität St.Gallen (HSG), Leading House for the Latin American Region

November 2022
Trainer used in sessions at University of Basel.

2. August 2021
First successful prototype of open source cleft surgical simulator .
This project supported by SNSF aims to develop algorithms for 3D modelling and simulation of infant face and head in collaboration with the Computer Graphics Laboratory at ETH Zürich.
The medical applications of the developed state-of-the-art AI-based pipeline are explored in craniofacial malformations found in infants and toddlers such as positional cranial deformities, orofacial clefts and craniosynostosis.

Speech Development in Children with Cleft Lip and Palate
Swisscleft Speech Outcome Measurement: National Multicenter Comparison
Literature and presentations at European cleft congresses show that associations and projects have been developing and evaluating standardised speech assessments and treatment protocols for quite some time. Systematic reviews are often regarded as the highest level of research evidence for implementing best evidence-based practice.
In Switzerland, the speech therapy protocols are collected individually in each of the Cleft Lip and Palate (CLP) centers. In the spirit of cooperation for a common outcome measurement, the clinics USB - University Hospital Basel, HUG – Hôpitaux Universitaires de Genève and Insel - Inselspital Bern have joined forces as a pilot project under the leadership of the USB to develop a Swisscleft Outcome Measurement as a standardised tool which can be used as a template for speech therapy diagnostics as screening in the CLP consultation.
The following codes and scales are collected and evaluated as uniform key data:
- ICD code
- LAHSHAL-Code (L=Lip, A=Alveolus, H= Hard palate, S=Soft palate)
- NAVSOM scaling with designation of severity (N=Nasality, A=Articulation, V=Comprehensibility, S=Voice, O= Orofacial myogene insufficience, M=Mimic movement)
The aim is to evaluate the collected data quantitatively and qualitatively both within the clinic and in direct comparison between the centers.



This research is performed in conjuction with the Department of Paediatric Oral Health and Orthodontics, University Center for Dental Medicine UZB, Basel https://www.uzb.ch/
We exploit in an in-silico study the potential of magnetic forces to stimulate the combined bone- and soft tissue formation by periostal distraction. This aims to recapitulate the natural process of cleft fusion as it should have happend during the development.
The in-silico study produced promising results. It further allowed to identify the ideal magnetic force which can now be applied in the following in-vivo anmial studies.
Nalabothu P, Verna C, Benitez BK, Dalstra M, Mueller AA. Load Transfer during Magnetic Mucoperiosteal Distraction in Newborns with Complete Unilateral and Bilateral Orofacial Clefts: A Three-Dimensional Finite Element Analysis. Appl. Sci. 2020;10(21):7728. https://doi.org/10.3390/app10217728

Microsurgical reconstruction is an important field and powerful technique for soft- and hard tissue reconstruction in the craniofacial region.
To evaluate current clinical practice, we aim to define goals for prospective trials and look for existing standards in clinical routine.
The questionnaire study covered a wide range of controversial topics, where no consensus and no evidence-based recommendation have been available.
The perfect intraoperative technique has been considered to be the single most decisive factor (mean score 6.0 worldwide (6.2 EU, 5.8 Germany) on a scale from 1 (not important) to 7 (very important)), followed by continuous postoperative monitoring (mean score 4.9 worldwide (5.2 EU, 4.3 Germany)) with only low perceived effectiveness of administered supportive medication (mean score 3.0 worldwide).
Kansy K, Mueller AA, Mücke T, Koersgen F, Wolff KD, Zeilhofer HF, Hölzle F, Pradel W, Schneider M, Kolk A, Smeets R, Acero J, Haers P, Ghali GE and Hoffmann J. A worldwide comparison of the management of surgical treatment of advanced oral cancer. J Cranio-MaxillofacialSurg. 2018;46(3):511-520. https://doi.org/10.1016/j.jcms.2017.12.031
Kansy K, Mueller AA, Mücke T, Koersgen F, Wolff KD, Zeilhofer HF, Hölzle F, Pradel W, Schneider M, Kolk A, Smeets R, Acero J, Haers P, Ghali GE and Hoffmann J. A worldwide comparison of the management of T1 and T2 anterior floor of the mouth and tongue squamous cell carcinoma – Extent of surgical resection and reconstructive measures. J Cranio-MaxillofacialSurg. 2017;45(12):2097-2104. https://doi.org/10.1016/j.jcms.2017.09.012
Kansy K, Mueller AA, Mücke T, Koersgen F, Wolff KD, Zeilhofer HF, Hölzle F, Pradel W, Schneider M, Kolk A, Smeets R, Acero J, Haers P, Ghali GE and Hoffmann J. Microsurgical reconstruction of the head and neck region: Current concepts of maxillofacial surgery units worldwide. J Cranio-MaxillofacialSurg. 2015;43(8):1364-1368. https://doi.org/10.1016/j.jcms.2015.06.034

Regenerative medicine strategies by use of biomaterial scaffolds and cellular components.
We explore alternatives to bone graft in developing bone tissue engineeering to regenerate bone.
- use of mesenchymal stem cells isolated from adult tissues for bone repair
- use of human umbilical cord in newborns as a source of mesenchymal stromal cells for bone regeneration in cleft patient treatment
- use of biodegradable polymers as auxiliary material for the functional and structural restoration
Naudot M, Barre A, Caula A, Sevestre H, Dakpé S, Mueller AA, Devauchelle B, Testelin S, Marolleau JP, Le Ricousse S. Co-transplantation of Wharton’s jelly mesenchymal stem cell-derived osteoblasts with differentiated endothelial cells does not stimulate blood vessel and osteoid formation in nude mice models. J Tissue Eng Regen Med. 2020;14(2):257-271. https://doi.org/10.1002/term.2989
Mueller AA, Forraz N, Gueven S, et al. Osteoblastic differentiation of wharton jelly biopsy specimens and their mesenchymal stromal cells after serum-free culture. Plast Reconstr Surg. 2014;134(1):59e-69e. DOI: 10.1097/PRS.0000000000000305
Mueller AA, Rahn BA, Gogolewski S, Leiggener CS. Early dural reaction to polylactide in cranial defects in rabbits. Pediatr Neurosurg. 2005;41(6):285-291. https://doi.org/10.1159/000088730

In order to overcome limitations of the conventional bone cutting instruments, we have developed a stand-alone robot-guided laser system, “Cold Ablation Robot-guided Laser Osteotome” (CARLO®), in collaboration with a Swiss spin-off company (Advanced Osteotomy Tools – AOT) from the Department of Biomedical Engineering at the University Basel. This system is constructed to allow direct collaboration of man and machine by means of a small, lightweight, and custom-designed tactile robotic arm, as well as navigation and control software and its corresponding hardware. These elements are combined in an ergonomic system to fit easily into the operating room and to allow the surgeon full control over this universal osteotomy device at any time. CARLO® is the world’s first medical, tactile robot that can cut bone without contact and with cold laser technology.
Advantages of CARLO® include but not limited to:
- Use of robotics with integrated navigation system results in autonomously performed hard tissue osteotomy, eliminating manual maneuver by the surgeons
- Contact-free osteotomy achieved by the use of an Er:YAG laser transcends the geometrical limitations faced by conventional methods
- Very accurate translation of the digital preoperative plan into the operating room, eliminating the need for a cutting guide
- Intraoperative adjustments of the planned osteotomy line made possible by the software of the CARLO® device
- Excellent healing potential due to the absence of thermal damage, preservation of trabecular bone structure and migration of cells to the edge of the osteotomy line
The First-in-Human trial has been completed to assess the safety and accuracy of the CARLO® device:
Ureel M, Augello M, Holzinger D, Wilken T, Berg BI, Zeilhofer HF, Millesi G, Juergens P, Mueller AA. Cold Ablation Robot-Guided Laser Osteotome (CARLO®): From Bench to Bedside. J. Clin. Med. 2021, 10(3), 450; https://doi.org/10.3390/jcm10030450
Holzinger D, Ureel M, Wilken T, Mueller AA, Schicho K, Milles G, Juergens P. First-in-man application of a cold ablation robot guided laser osteotome in midface osteotomies. J Cranio-Maxillofac Surg. 2021; https://doi.org/10.1016/j.jcms.2021.01.007

We are interested in the well being of infants undergoing surgery, as well as of children and adolescents with cleft lip and palate. We study including the following aspects:
- As a clinical routine, we perform patient reported outcome measurements (PROM) according to the International Consortium of Health Outcome Measurements (ICHOM). In 2020 we have translated the standard questionnaire of the McMaster University (Cleft-Q) into German. It is free to non-profit users.
- psychological psychological functioning, interactional competencies, quality of life, and sleep patterns among children, adolescents and adults with orofacial clefts
- sleep patterns and cortisol secretion in infant during surgeries
Find more about:
Cleft-Q
http://qportfolio.org/cleft-q/
PROM
https://saez.ch/article/doi/saez.2018.17187
ICHOM cleft
https://www.ichom.org/resource-library/category/condition-specific-resources/cleft-lip-palate/
Mueller AA, Kalak N, Schwenzer-Zimmerer K, Holsboer-Trachsler E, Brand S. Cortisol levels and sleep patterns in infants with orofacial clefts undergoing surgery. Neuropsychiatr Dis Treat. 2014;10:1965-1972. https://doi.org/10.2147/NDT.S71785
Brand S, Blechschmidt A, Mueller AA, Sader R, Schwenzer-Zimmerer K, Zeilhofer HF and Holsboer-Trachsler E. Psychosocial functioning and sleep patterns in children and adolescents with cleft lip and palate (CLP) compared with healthy controls. Cleft Palate-Craniofacial J. 2009;46(2):124-135. https://doi.org/10.1597/07-165.1
Current and past funding agencies